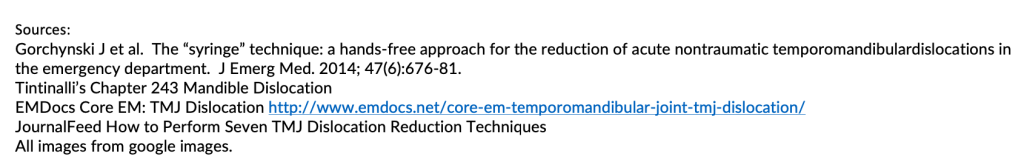
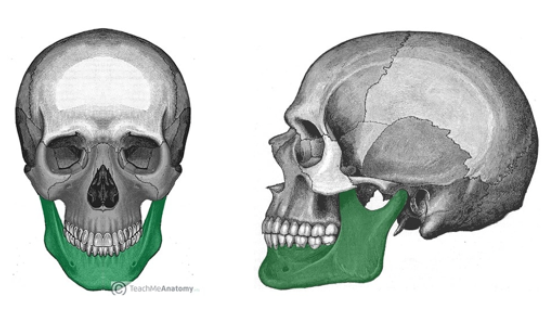
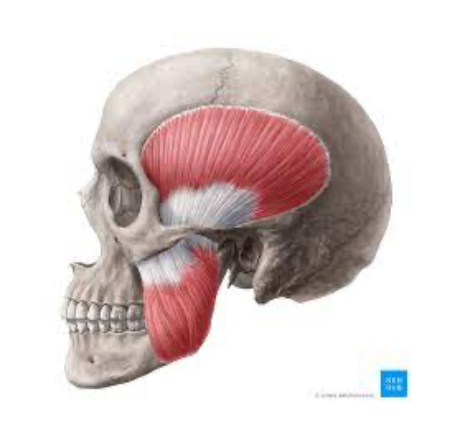
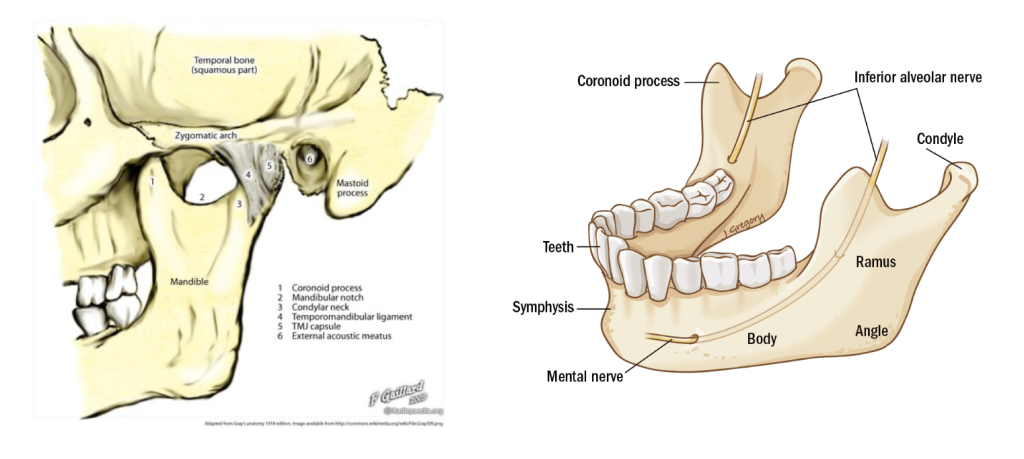
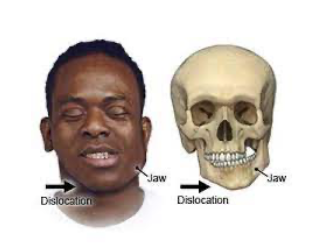
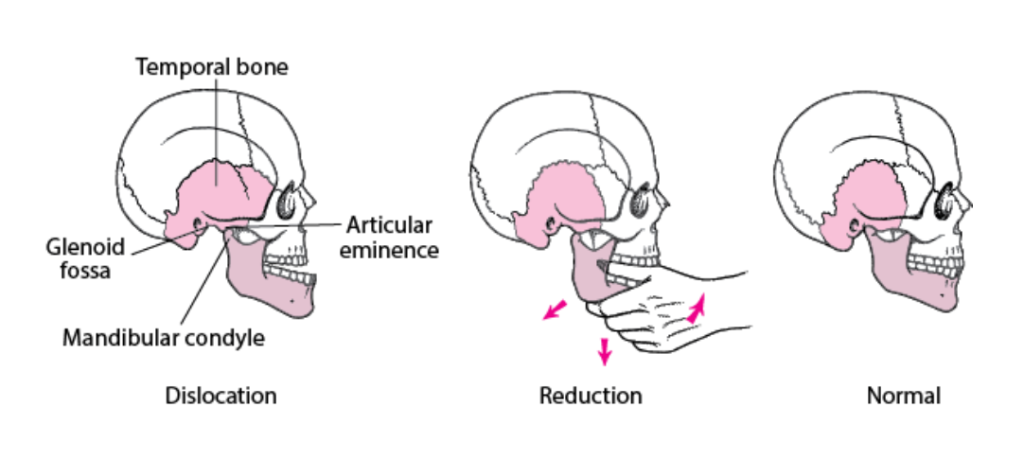
Let’s talk about mandible dislocations & how we can reduce them. First, we need to take a look at the mandible anatomy – can refer back to this as we discuss mandible dislocation:
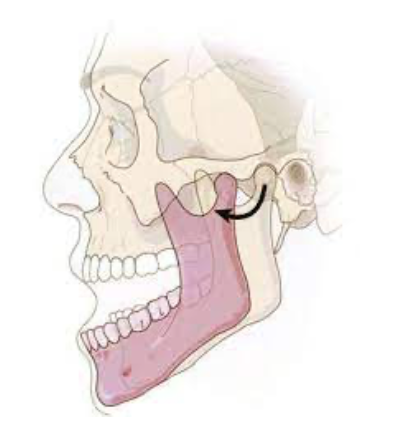
So how does the mandible dislocate (also called temporomandibular joint dislocation)?
Causes:
- Often due to trauma – direct blow
- Can break condylar neck w/ dislocation
- Lateral dislocations often w/ fracture
- Check for loose or missing teeth!
- Iatrogenic: ex. dental extraction, tonsillectomy, general anesthesia (the case I saw had happened during endoscopy)
- Seizure
- Spontaneous ex. with laughing, yawning, vomiting, even taking large bite of food!
- Prior mandible dislocation = increased risk for recurrence
- Dislocation Location:
- Usually bilateral but can be one side
- Anterior = most common: mandible condyle forced out
- Posterior, superior, & lateral: severe trauma
- Posterior = rare
- Superior = bad: blow to partially open mouth > condylar head upward > badness – can have associated cerebral contusions, facial nerve palsy, deafness
- How does the mandible get stuck there?
- Muscle spasm traps mandible out of position- strong & mighty temporalis & lateral pterygoid muscles make reduction difficult
- Symptoms: severe pain, difficulty speaking or swallowing
- Anterior pain often right in front of tragus
- Can have sensation loss part of chin or mouth
- Signs:
- Prominent lower jaw (in anterior), difficulty moving jaw
- Palpable depression preauricular from displaced mandible condyle
- If unilateral: jaw deviates away from dislocation
- In posterior: condylar head can prolapse into auditory canal: examine external auditory canal & confirm hearing baseline
- Diagnosis:
- Clinical for the cooperative patient w/ spontaneous (atraumatic) anterior dislocation
- Any trauma: CT max/face first – eval for fracture
Now that we know mandible is out, can we reduce it? There are several different techniques we can use:

For closed anterior dislocation without fracture: reduce in ED ourselves
Superior or open dislocations or associated fracture: do not reduce it. consult ENT (or max-face surgeon depending on who is covering).
Setup:
- Airway & hemodynamic monitoring
- Can give short-active IV muscle relaxant like Versed: reduce muscle spasms
- Full procedural sedation might be required to overcome muscle spasms
- propofol = great choice – muscle relaxant effect
- Alternative: local anesthesia: small-gage needle into preuauricular depression just anterior to tragus – inject 2 cc’s of 2% lidocaine
Anterior dislocation reduction: A few different techniques:
Syringe technique= the lazy way: patient gently bites down & rolls 5 or 10 cc syringe back & forth using top & bottom molars on affected side > gliding motion, mandible slides posteriorly
- Can always try this one first but may need to move on to more forceful technique
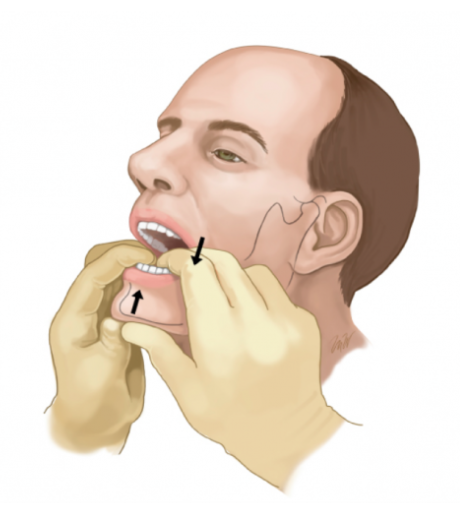
Conventional method = most common technique:
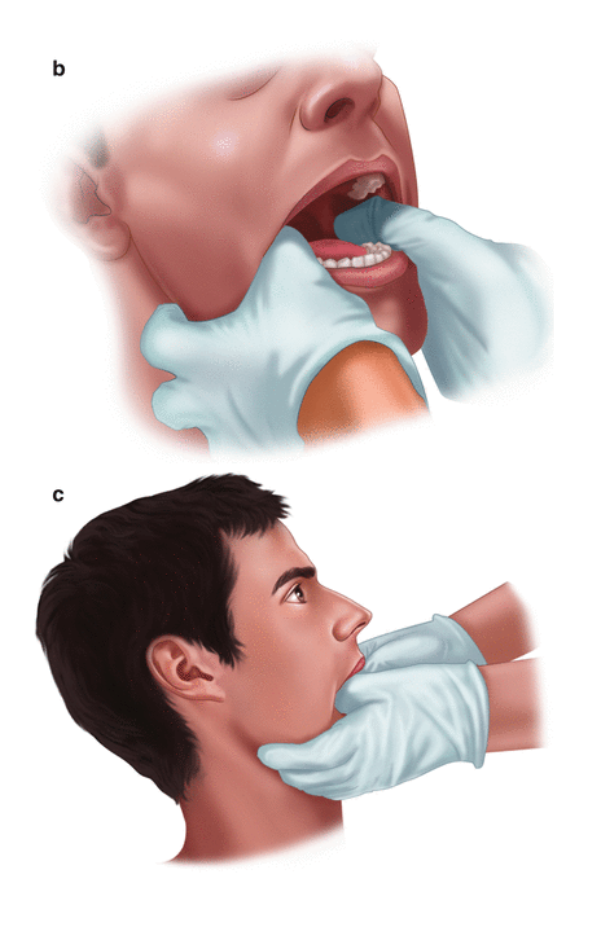
- Patient seated w/ head against wall or seat back
- Cushion: tongue depressor on each side or layers of gauze
- Your elbows at mandible level
- Facing patient place gloved thumbs in mouth over lower molars as far back as possible
- Curve fingers beneath angle & body of mandible
- Apply thumb pressure downward & backward (toward the patient)
- Slightly opening the jaw may help disengage it
- Use STRONG pressure – jaw muscles are VERY strong! & you will have to overcome them
- Sometimes easier to relocate one side at a time if bilateral
Alternate methods:
- Patient supine, stand at head of bed & thumbs on molars, downward & backward pressure (toward stretcher)
- Wrist pivot method: patient & provider sit. Instead of thumbs on molars, fingers on molars & thumbs on chin, thumbs push up on chin while fingers push down on lower molars, wrist flexes, & mandible rotates into position
- One randomized controlled trial found wrist pivot method w/ highest success rate
- Extraoral method: patient seated, you in front of patient, thumb on cheek – ramus & coronoid process of dislocated side, then apply persistent posterior pressure. Fingers placed behind angle of mandible to stabilize grip. At same time on opposite side: fingers of other hand on angle of mandible & pulls towards you. Note that this causes further anterior dislocation on that side, rotates the jaw, & allows other side to be reduced.
- Once one side reduced, other side often goes back spontaneously. If not, repeat on opposite side w/ minimal force to reduce 2nd side.
- Another option: posterior force on both coronoid processes at the same time if above doesn’t work.

Unable to reduce? Get ENT involved.
Able to reduce – That jaw drop is fixed! Now what?
- Know it’s successful when: patient able to easily close mouth
Post-reduction care:
- No need for post-reduction imaging unless: reduction difficult or traumatic, or significant pain after
- Complications = rare. Include fracture or articular cartilage avulsion
- Disposition: after successful reduction can discharge home
Discharge instructions:
- Soft diet
- Don’t open mouth >2 cm x2 weeks
- Support mandible w/ hand when yawning
- NSAIDs for pain
- Outpatient elective referral to oral max-face surgeon; severe cases may need intermaxillary fixation to control jaw motion during healing
- Chronic dislocations may need operative intervention
Now you know how to diagnose & manage mandible dislocation! Jaw drop fixed!